Antibiotics: Are they bad for you?
"My family physician wants me to take another antibiotic for this cold that won’t go away, but I have read that antibiotics may damage my gut and may even make me put on weight,” a client asked me just the other day. “I’ve read conflicting reviews, and I know you’ve warned me against them in the past, but really, how bad are antibiotics?”
Firstly, let’s not entirely dismiss antibiotics. After all, they can be life-saving and in particular, circumstances, very necessary. Since they were first developed, they have saved millions of lives. Believe me, we do not want to live without antibiotics.
That being said, antibiotics now are over-prescribed and frequently unnecessary. Advancements to prevent and treat infectious diseases – like sanitation, vaccines and best use of antibiotics – have significantly decreased deaths from infectious disease. But there is a cost.
Consider sanitation
Hyper-focusing on hygiene and sterilization by using hand sanitizers has dramatically changed our gut bacteria, spiking autoimmune diseases and contributing to conditions like obesity, diabetes, heart disease, depression and autism.
Although western medicine has considerably advanced with the treatment of acute disease, it has bombed miserably treating chronic illness.
One bug, one disease, and one drug
Louis Pasteur observed bugs cause infections, and Alexander Fleming invented antibiotics to kill them. This simple cause and effect “cure” – one bug, one disease, and one drug – may work for infection, but not at all for chronic illness.
Since that point, scientists have been looking for “cures” for chronic diseases (including cancer and dementia), but still after millions of dollars, they can’t find them! Modern Medicine’s goal has become the hunt of a holy grail — a drug for every ill. This failed strategy will continue to flounder because chronic disease results from the complicated interplay of our genes, lifestyle and environment. A magic tablet or just isn’t going to cure us. We require a holistic, robust lifestyle approach.
 So let's get back to the original question
So let's get back to the original question
Antibiotics can become harmful because they destroy your friendly bacteria, what scientists collectively call our microbiota, which is composed of 100 trillion microbes that live inside you and outnumber your cells an astonishing 10 to 1.
It is true, antibiotics clear out the harmful bugs that are causing the infection; but they are like napalm, annihilating everything in their path including the good bacteria.
That becomes a real issue because these bacteria collectively contain at least 100 times more genes than you do. That bacterial DNA in your gut exceeds your DNA by a huge margin.
This fact is critical, because, among its roles, this bacterial DNA regulates immunity, governs digestion and intestinal function, defends against infections and even produces vitamins and other nutrients.
Antibiotics destroy these beneficial bacteria, which also encourages the overgrowth of harmful bacteria, fungus, and candida, leading to many problems including depression, food sensitivities, tiredness, skin issues and of course, digestive problems.
Sugar Cravings and Weight gain
Overgrowth of harmful bacteria can also encourage sugar cravings contributing to weight gain and other problems that eating sugar creates. So it is evident that antibiotics can probably make you fat.
When a client first comes to see me, I always ask them when they have had to take antibiotics in the past. More often than not, taking antibiotics has been the triggering event for the start of their current health issues.
I recently had a client born by C-section, who was then bottle fed, and as a child suffered recurrent ear infections. Her family doctor Conventional doctor, doing what they have taught prescribed antibiotics, which ultimately lead to irritable bowel syndrome during the client's teenage years, and then Rheumatoid arthritis as a young adult. I hear this story regularly, and much of this originates from not valuing, respecting and tending to your microbiota.
More often than not, the antibiotics our children are prescribed for ear and throat infections, for which they probably would have gotten better on their own, have ruined their fragile gut bacteria beginning at an early age.
What the latest research is saying about antibiotics
A study, by the Centers for Disease Control and Prevention (CDC), found that 71 percent of a group of children who suffered from a Clostridium difficile infection took many rounds of antibiotics for chest, ear, nose and throat illnesses 12 weeks before infection.
Another study published in The American Society for Microbiology found a one-week course of antibiotics could negatively affect your microbiome for a whole year.
Other studies link long-term antibiotic use to various problems including depressed immunity, raised stress levels, behaviour issues and obesity.
While antibiotics can occasionally be necessary, I highly recommend if your family physician offers you antibiotics ask them if them whether there are any alternatives including allowing infections to heal on their own. If you are not happy with their response, then I suggest seeking out a Functional Medicine practitioner or Naturopathic Doctor who are expert in such matter.

If it is necessary that you take antibiotics, such as when you have a kidney infection, I highly recommend a few steps before and after using them:
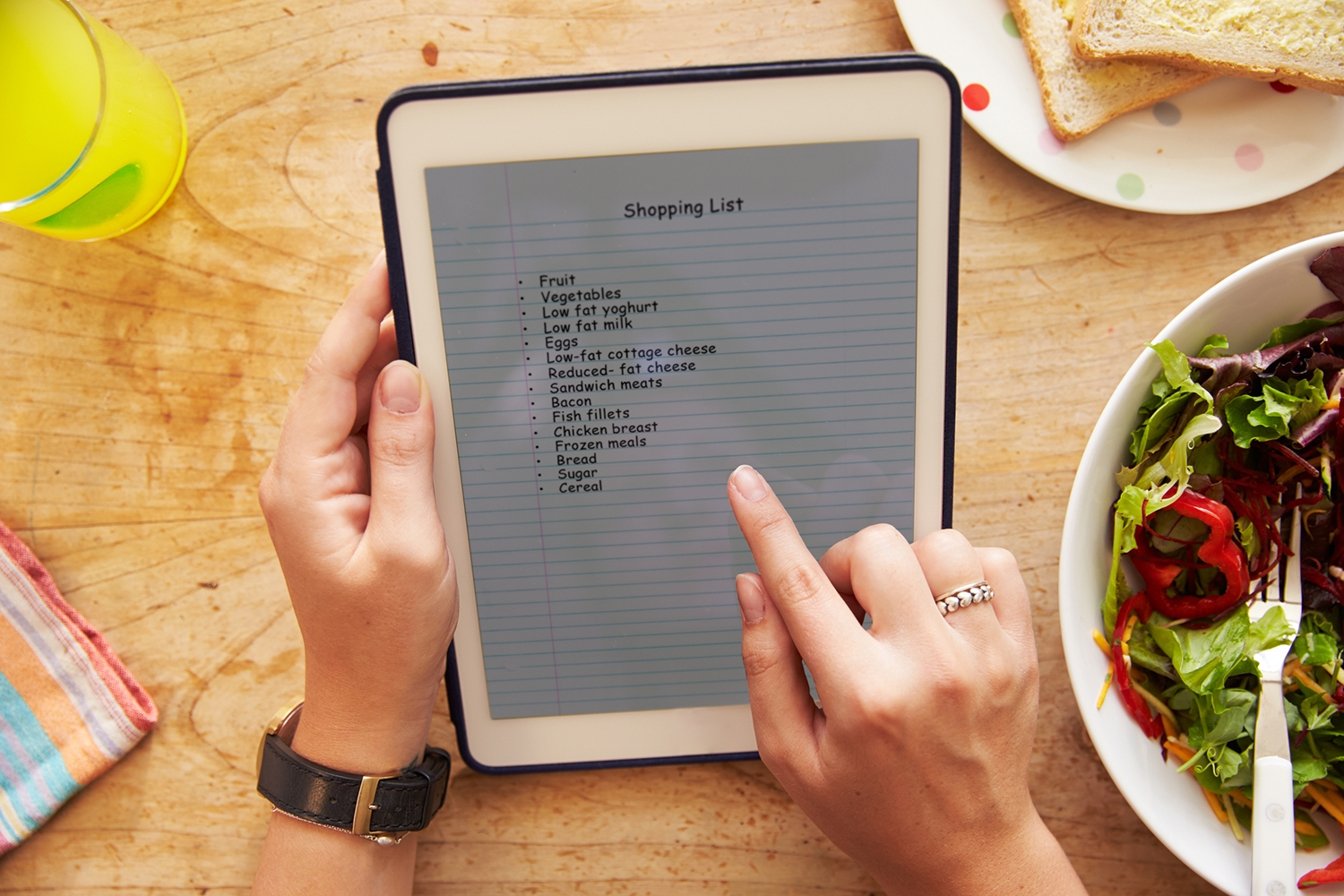
Step 1: Feed your good bacteria
- Eat a low-glycemic, whole-foods diet.
- Take quality probiotic. A high-quality, multi-strain probiotic will help populate your gut with beneficial bacteria. Prebiotics, a form of soluble
- Consume prebiotics. Prebiotics a kind of soluble fibre, found in onions, garlic, resistant starch such as potato starch, sweet potatoes, dandelion greens and jicama, will help feed your good bacteria.
Contrary to regular starch, your small intestine doesn’t digest potato starch. Instead, your gut bacteria break it down it, producing compounds that help balance blood sugar and healthy gut bacteria. My favourite resistant starch is Bob’s Red Mill Unmodified Potato Starch. I recommend adding about one teaspoon to a glass of water.
Step 2 – Repair Your Gut (especially after you’re finished using antibiotics)
- Take gut-healing nutrients such as L-glutamine, omega-3 fats, vitamin A and zinc to repair your gut lining.
- Use of digestive enzymes to help you digest your food better.
Have ever taken antibiotics? Did you use prebiotics, probiotics, resistant starch, or other supplements to help heal your gut? Did you suffer any unfavourable consequences from antibiotics? Share your story below.