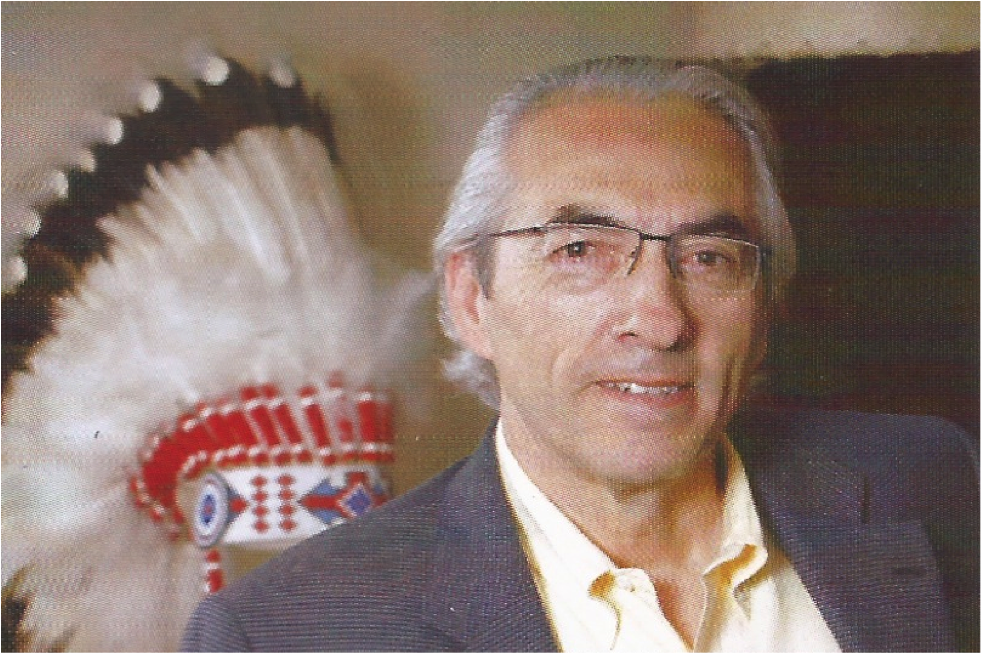
From poverty to wellness — Interview with AFN National Chief Phil Fontaine
Take a close look at some recent I statistics for First Nations. Overcrowded, modest houses crammed with multiple families abound. There is mould growth and unsafe drinking water in 44% of homes. Tuberculosis rates are 29 times higher than that of others born in Canada; life expectancy on average is between five and seven years less than everyone else plus there are higher levels of asthma, rashes and allergies in children. Moreover, another statistic that is particularly poignant, population growth for First Nations is booming to the tune of about double the Canadian average. Absent of change and with an increasing population, these health issues will become a larger problem for First Nations and Canadian society as a whole.
AFN National Chief Phil Fontaine
The March report, The State of the First Nation Economy and the Struggle to Make Poverty History, declared that "in 2009, First Nations communities are still, on average, the most disadvantaged social/cultural group in Canada on a host of measures including income, unemployment, health, education, child welfare, housing and other forms of infrastructure."
There is no question that there is a significant correlation between socio-economic status and health. It is true the world over, across all societies and populations, that the economically disadvantaged have poorer health.
Canada's First Nations are no exception and as Assembly of First Nations National Chief Phil Fontaine explains, the situation for First Nations is compounded by two factors unique to First Nations communities: "inter-jurisdictional barriers to health care and inequitable funding."
First Nations are one of a handful of groups in Canada that receive their health care directly from the federal government. The First Nations and Inuit Health Branch of Health Canada has an annual budget in the range of $1.8 billion, which serves over 700,000 First Nations clients and 40,000 Inuit clients. While it may sound simple, it isn't. As Fontaine points out, "First Nations patients often have to deal with three health jurisdictions: federal, provincial/territorial and First Nations. When health care systems don't work together, patients fall through the cracks."
Take the astonishing case of Jordan Anderson. Jordan, who died when he was five, spent his whole life in a hospital, not because he was too sick to leave but because of inter-jurisdictional squabbling over who would foot the bill for his care if he returned to his community. A recent study found close to 400 such cases of kids caught in such jurisdictional disputes.
Currently, Fontaine says, there are steps being taken to address this issue by Health Canada through a cross-jurisdictional policy framework allowing First Nations to become full partners with federal and provincial governments. This will definitely improve the situation but the point stands that these are issues that non-First Nations Canadians (of any income bracket) just don't have to worry about.
More funding and better coordination are part of the solution to improve the wellbeing for First Nations, but as in every other sector of society, innovation rules and First Nations are brimming with innovative ideas just waiting to be tapped. Fontaine points to the Bigstone Cree First Nation as an excellent example of how First Nations can improve their own health care. "The Bigstone Cree First Nation is a remote community approximately 400 km north of Edmonton and consists of seven settlements, Fontaine says, "It has an impressive Health Centre that contains medical offices, a dental clinic and a pharmacy. The pharmacy not only creates employment but it generates profits that the community reinvests in health care."
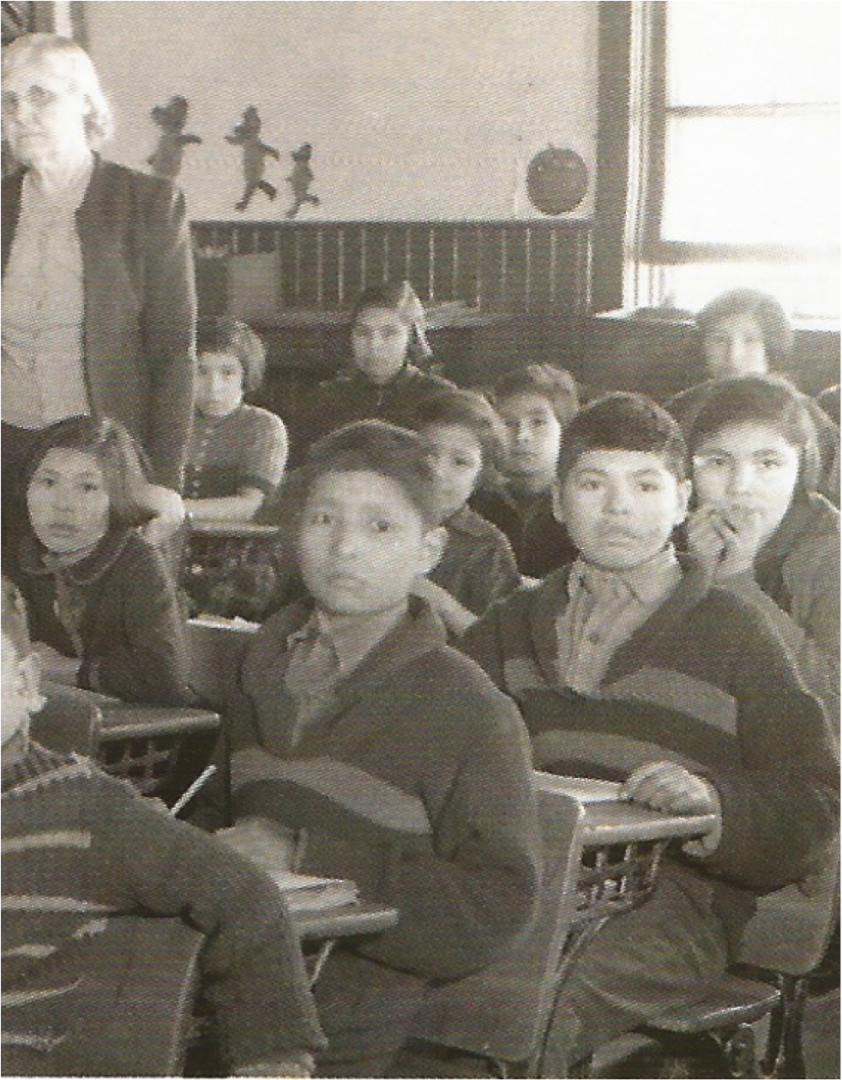
Investing in education is another extremely compelling way to improve quality of life and health for First Nations. "Education provides hope and opportunity," says Fontaine. "Part of the problem we encounter with education that fuels the dropout rate is the fact that we are not investing a fair amount in First Nations education."
According to the AFN, 42 First Nations do not actually have schools and twice as many have schools that are in terrible disrepair. On average, First Nations schools receive $2,000 less per student in educational support than students in provincial schools, which clearly puts them at a disadvantage.
Improve education and health will follow. From the engaged, educated youth will come health care professionals from the region and as Fontaine underlined, according to a 2004 report by the Canadian Medical Association, health professionals from remote communities often return to these areas to practice. This could only be good news for the future of First Nations communities — on many different levels.