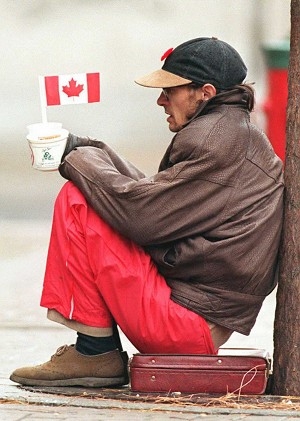
The Great Canadian Experiment to House the Homeless
That health is more than health care was a point I heard many times on my recent Fulbright fellowship visit to Canada. Right now in the U.S., you’d never know that though, what with all the hullaballoo over dysfunctional websites and failed efforts to get more people covered by insurance. You’d think the only thing that matters is a cheap premium that somehow equates with good health outcomes.
Well, all Canadians have access to health care, but not every Canadian has good health, and on this trip I heard much more about the social determinants of health than about the country’s infamous waiting lists. When I asked Canadian health expert Michael Decter, who served as a deputy health minister in Ontario, what his top priority was for Canadian health care, it wasn’t reducing wait times for cataract surgery. It was addressing the poor health of the country’s Aboriginal populations, which he called an embarrassment. “To fix this”, he said, “the country must deal with poverty, diet, education and housing.”
In the U.S. we don’t often think about coupling housing with health, but Canada has. One project, At Home/Chez Soi, funded by the Canadian government, is a randomized controlled trial focused on housing for the mentally ill. At Home/Chez Soi is built around the concept that housing is the first order of business, and then comes support services that honor a person’s choices and offer a range of resources, says Dr. Paula Goering, a psychiatry professor at the University of Toronto who led the study.
At Home/Chez Soi provides housing to the mentally ill who need it to re-enter society, Goering noted in a post that she and colleague Stephen Hwang wrote for EvidenceNetwork.ca (a repository of studies that examine the evidence for various health policy interventions). They wrote that traditional housing solutions for the homeless, such as community programs and beds in shelters, “have not measurably reduced the number of homeless people country-wide,” so the Canadian government looked for other cost-effective alternatives. “People don’t like to live in group homes,” Goering told me when I visited with her in Toronto a few weeks ago.
Some 2,250 homeless people in five Canadian cities enrolled in the program in 2011. Half of them received mostly private-sector housing; the other half got the usual community or shelter referrals. Those in the private sector group chose an apartment in a neighborhood they liked, and the program provided the furniture. Participants contributed 30 percent of any monthly income they received toward the rent while subsidies from At Home/Chez Soi paid the remainder. They also had to agree to a weekly visit from a case manager.
To qualify for this housing initiative, individuals don’t need a job or a stable lifestyle, and they don’t need to enter rehab Goering and Hwang wrote. However, those who had their own apartments started asking for additional help to keep their home and the stability, privacy and safety it offered, Goering noted.
What are the results so far? For people in their own apartments, “the quality of life is better and aspects of social functioning are better,” Goering explained. “And they are using more services in the community than acute services.” That could be a plus given that Canada is trying to shift care from costly acute care settings to care in the community, which frees up resources for the very sickest and trims wait times for elective surgeries. There is some evidence, Goering added, that use of emergency rooms is down, too.
While researchers expected to see different physical and mental health outcomes for the two study groups, they found improvement in both. The reasons: perhaps some participants who were in crisis at the beginning of the study returned to a more normal state anyway, or maybe the similar effects stem from what Goering calls “an accessible health care system that does serve both populations.”
On the money side, the interim results point to cost offsets for other services. Goering added that “for every ten dollars spent on housing, seven dollars are saved in health and criminal justice costs.” Researchers in Portugal, Australia, and France have looked at the program, and the French have started their own parallel study. What’s next? The program is likely to continue with support from the federal government whose response to the project’s success has been “quick and dramatic.” Goering said the fact that the program was a randomized controlled trial strengthened researchers’ voice in government. They had also hoped for support from the cities and provinces to continue the program, but that has been slower to achieve. Funding has been secured in two cities, is somewhat in place for two more, but not at all in the fifth one, Montreal.
Still, At Home/Chez Soi is an innovative approach to homelessness that reinforces the truism that good health is more than swallowing the latest wonder drug.
Trudy Lieberman, a journalist for more than 40 years, is an adjunct associate professor of public health at Hunter College in New York City. She is a longtime contributor to the Columbia Journalism Review and blogs for its website, CJR.org, about media coverage of health care, Social Security and retirement. As a William Ziff Fellow at the Center for Advancing Health, she contributes regularly to the Prepared Patient Blog.









